If you know anything about grappling, then you have definitely heard about or seen cauliflower ear. Those who haven’t been involved in certain contact sports (e.g. wrestling, BJJ, rugby, etc) often have never heard of it. Interestingly, to the medical profession, it is deemed an uncommon malady. Yet it is a common concern I am asked about and treat among my jiu-jitsu team and if you ever hit an adult class at a BJJ gym, there’s no way you can miss seeing cauliflower ear. While there’s no research to definitively say why this disconnect occurs, my own experience is because it is very commonly treated outside the medical establishment. This leads to an underreporting of cases, and therefore the doctors who treat it come to think of and report cauliflower ear as an uncommon occurrence.
Despite the lay person’s ability to prevent cauliflower ear, there still is a bit of misperception about what causes it and how it arises. And despite the medical establishment not always being the first stop for treatment, the medical community does know quite a bit about the issue. In fact, as this article will discuss, it’s been around since antiquity. So, here’s a quick bite summary of cauliflower ear followed, for those interested, by the deep dive.
- Cauliflower ear is not a new phenomenon, and in fact it has been a documented affliction and sequelae of ear trauma for thousands of years.
- Cauliflower ear is actually disorganized regrowth of cartilage that occurs when a hematoma, i.e. a contained collection of blood often arising from trauma, is left untreated anywhere on the ear other than the ear lobe.
- The vast majority of cauliflower ear is preventable if the hematoma is drained and prevented from recurring.
Continue Reading: 10min Read
History
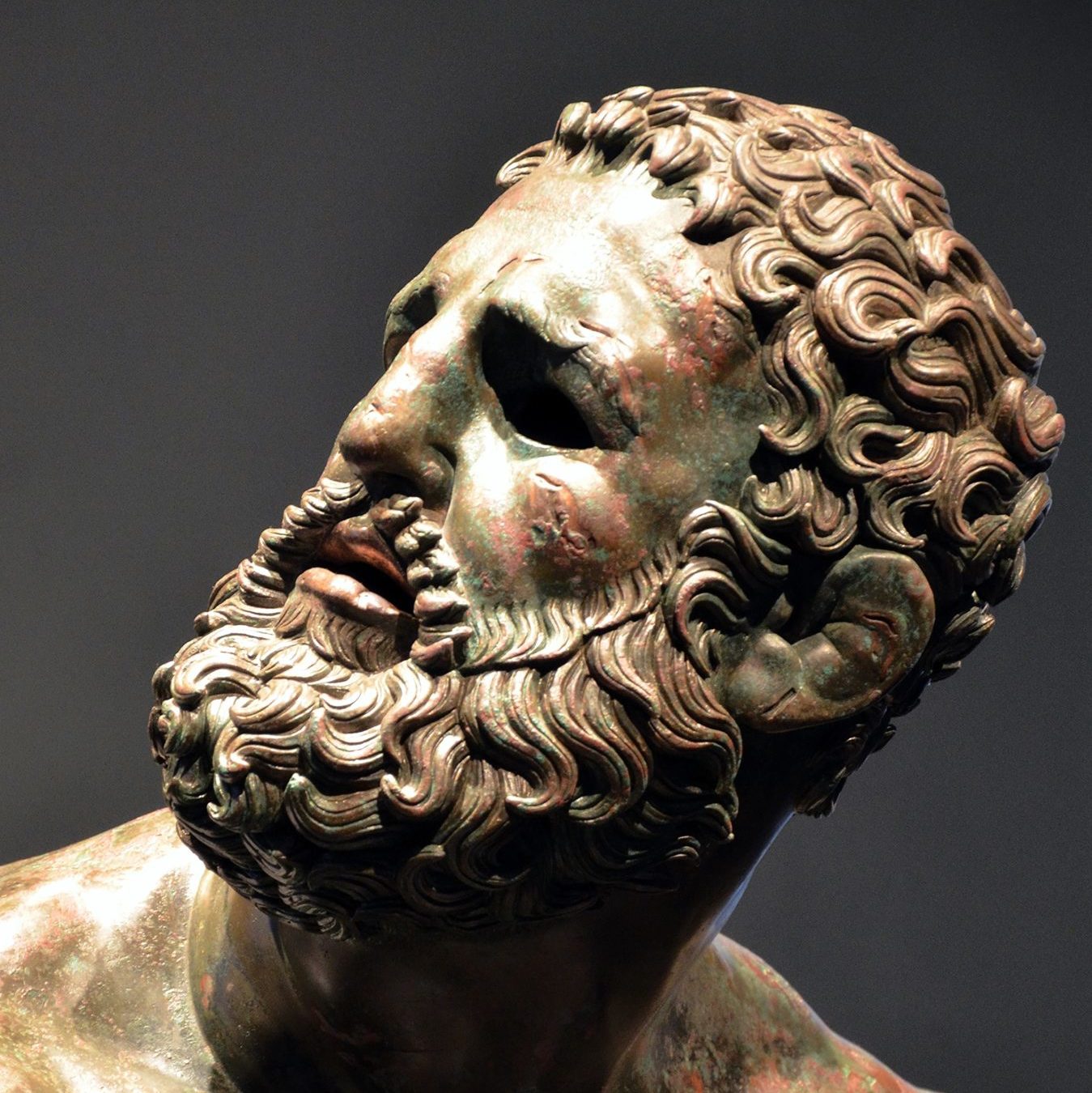
Cauliflower ear is not new. While documented medical science did not start discovering the details of its cause until the 19th century and researching its treatment until the 20th century, it has in fact been well known and documented for over 2 millennia. From documentation of Plato to works of art still intact today from the Hellenistic period (click on Figure 1 for more details), cauliflower ear has captured the minds and hearts of people through the ages.1
Also noteworthy is that the term cauliflower ear as common nomenclature is quite recent. Ancient Greek and Roman literature referred to it often as battled, broken, or bruised ear. Ear mushroom was a common term in the 2nd century while othematoma was more common in the mid 1800s. It wasn’t until about 1905 that the label of cauliflower ear became more common place.2
Anatomy and Physiology
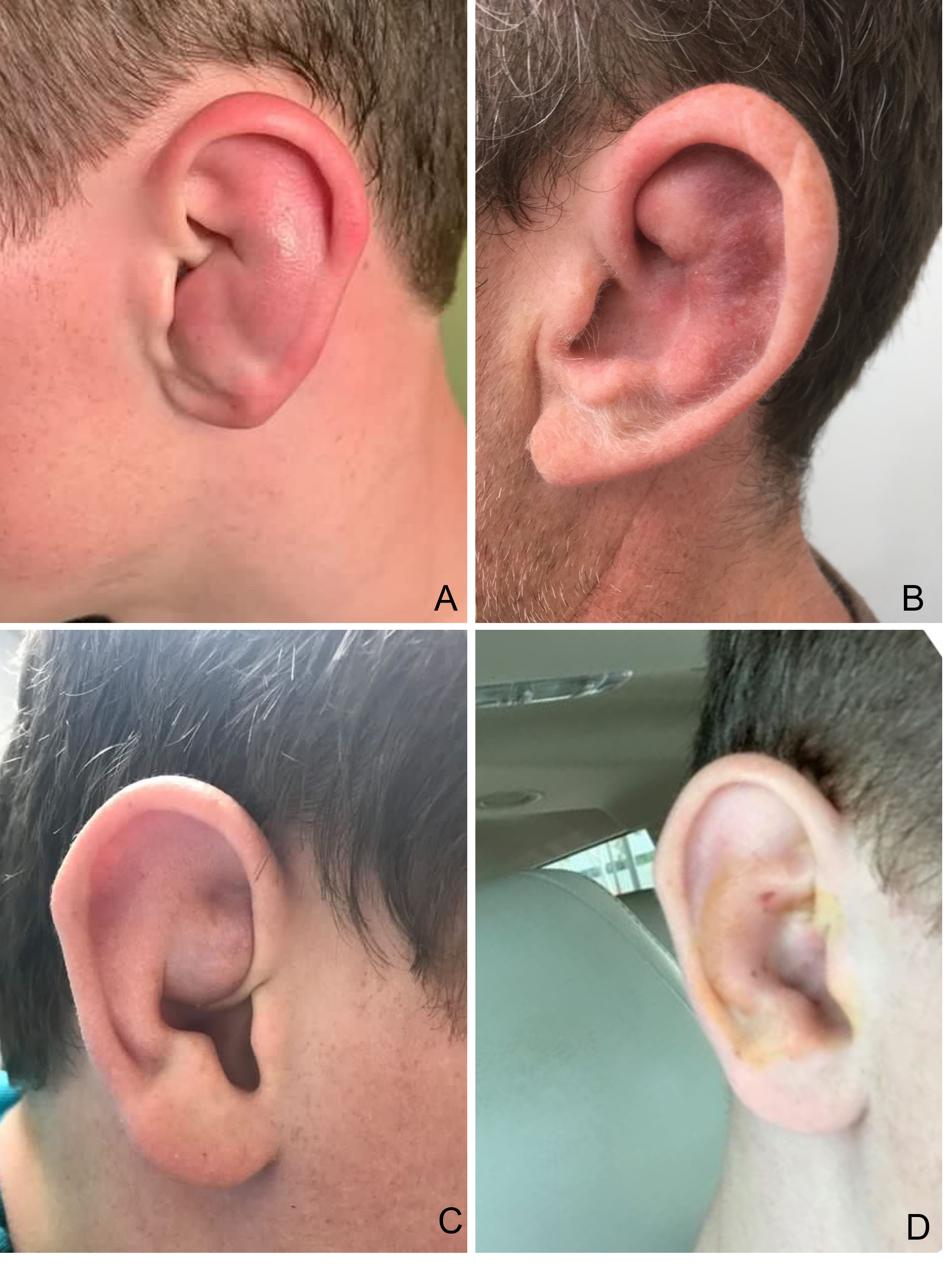
The visible external ear is mostly a cartilaginous structure with skin overlying it. The blood supply for the cartilage comes from a covering layer of tissue that lies between it and the overlying skin (a.k.a. perichondrium). If that blood supply is interrupted, then the affected cartilage will die, a process in medicine we call necrosis. It will then have a disorganized repair leading to scarring which is termed cauliflower ear (click on Figure 2). The most common interruption in the blood supply is a hematoma forming either between the cartilage and the perichondrium or in the cartilage itself, often from trauma to the ear.3, 4, 5
This is referred to as an auricular hematoma or sometimes a perichondrial hematoma (click on Figure 3). If the hematoma is drained and the skin and its perichondrium layer is realigned with the cartilage, then the process above is very unlikely to occur and the vast majority of cauliflower ear cases can be prevented.
Treatment
As alluded to above, the best way to treat cauliflower ear is to prevent it from even occurring.
First of all, wearing headgear significantly reduces trauma to the ear. But if one sustains ear trauma and gets an auricular hematoma, then the next best step is to drain it. Most auricular hematomas can be drained with a simple needle aspiration, but others (especially if >2 cm in size, if it recurs after aspiration, or if it has been there for more than 48 hours) will likely need a more involved procedure to not only evacuate the hematoma but to also leave a mechanism in place to prevent the hematoma from forming again.6
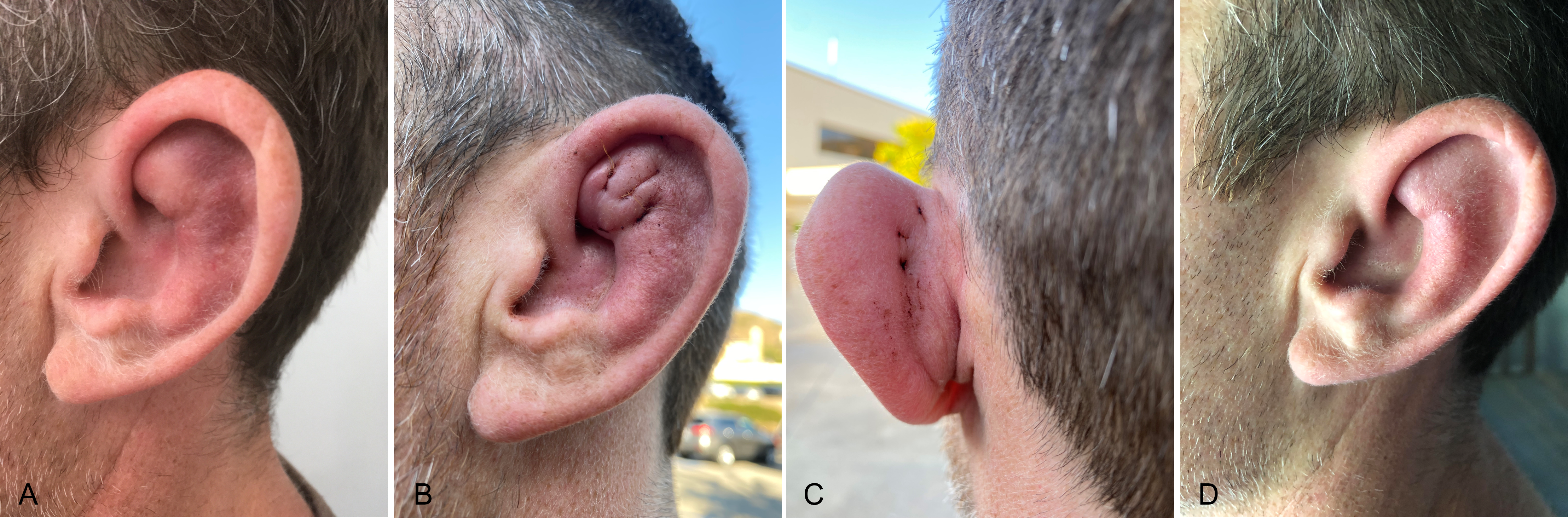
There are two methods a clinician can pursue that don’t involve leaving a compression mechanism, or bolster, in place after draining the hematoma. The first is gaining much traction among physicians recently as it allows athletes to return to sporting activity immediately and has had excellent outcomes. It involves making a small incision to drain the hematoma, leaving this incision site open while also tacking down the potential space of the hematoma with sutures to help keep that space closed (click on Figure 4). Another option after aspiration of the hematoma is to leave a a small catheter, such as a small IV catheter, to facilitate ongoing drainage.7,8,9,10
Figure 4 I&D with Suture Sequelae
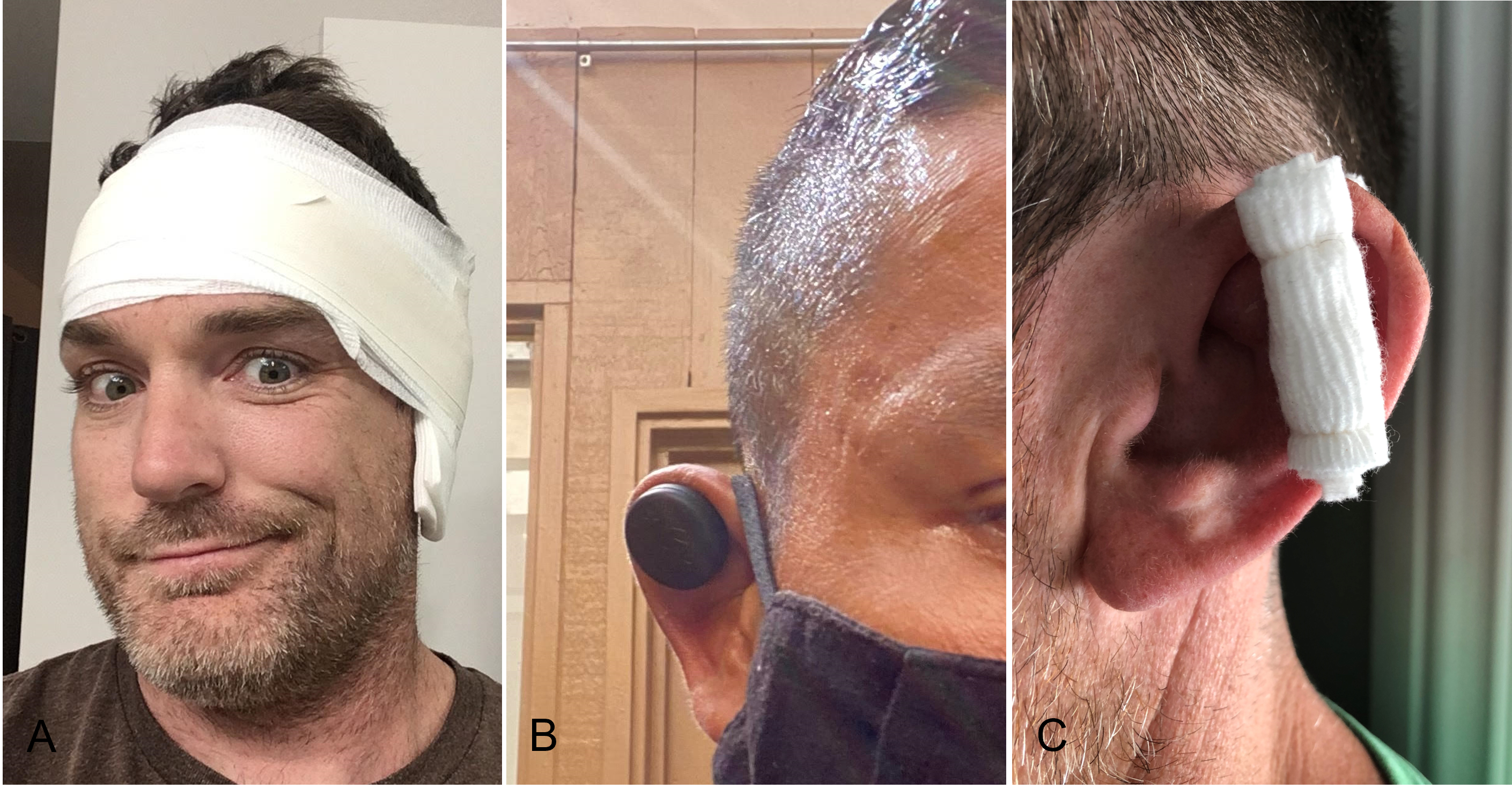
If one does not have access to a catheter or know how to do the above incision and drainage technique, other ways to try and prevent hematomas from recurring involve placing some sort of external pressure over the skin where the hematoma had been for two to three days after it is drained. This is known as a bolster. Most classically surgeons will sew rolls of gauze on either side of the ear. Some will apply a pressure bandage, with gauze padding either side of the involved ear, and a gauze roll then firmly wrapped around it and the entire head for counter pressure. Other modalities have been created, such as clips and magnetic discs that press the affected area of the ear like a pressure bandage would (click on Figure 5 for examples).
Figure 5 Bolster Examples
While studies have shown that evacuating the hematoma and preventing it from reforming do in fact prevent cauliflower ear from developing, the reality is that there have not been rigorous randomized clinical trials comparing the above methods to show which is the best and safest way of preventing hematoma recurrence. In the experience of most medical providers, hematomas <2cm in size and <48 hours old typically don’t recur after a simple needle aspiration so most don’t need anything further other than maybe a day of a bolster.11 However, other hematomas can have up to a 75% recurrence rate10 with this approach and so based on the medical literature, as well as my own experience both as a physician and with my own auricular hematomas, considering something more than aspiration alone if one encounters this situation is completely reasonable.
Conclusion
Conclusion
Cauliflower ear is not the swelling one has after an acute ear injury, it’s the (usually) permanent sequelae of not dealing with the swelling when it’s from a hematoma. For those that want the look cauliflower ears give, let nature take its course. For those that don’t, you now have enough information to know how to prevent them from happening and still have a great and aggressive roll on the mat. A last word of parting advice: with ear trauma and any of the therapies above, it’s possible to introduce microorganisms where they shouldn’t be. In other words, if you notice spreading redness, swelling, increasing pain, or warmth then I definitely recommend having it evaluated by a medical professional as an infection could have occurred and you may need antibiotics to successfully treat it.
References
- Mudry A, Pirsig W. Auricular hematoma and cauliflower deformation of the ear: from art to medicine. Otol Neurotol. 2009 Jan;30(1):116-20. doi: 1097/MAO.0b013e318188e905. PMID: 18800018.
- Mudry A, Jackler RK. Tracing the Origins of “Cauliflower Ear” and Its Earlier Names over Two Millenia. Laryngoscope. 2021 Apr;131(4):E1315-E1321. doi: 1002/lary.29055. Epub 2020 Sep 5. PMID: 32888356.
- Ohlsén L, Skoog T, Sohn SA. The pathogenesis of cauliflower ear. An experimental study in rabbits. Scand J Plast Reconstr Surg. 1975;9(1):34-9. doi: 10.3109/02844317509022854. PMID: 1162288.
- Ghanem T, Rasamny JK, Park SS. Rethinking auricular trauma. Laryngoscope. 2005 Jul;115(7):1251-5. doi: 10.1097/01.MLG.0000165377.92622.EF. PMID: 15995516.
- Pandya NJ. Experimental production of “cauliflower ear” in rabbits. Plast Reconstr Surg. 1973 Nov;52(5):534-7. doi: 10.1097/00006534-197311000-00010. PMID: 4745576.
- Greywoode JD, Pribitkin EA, Krein H. Management of auricular hematoma and the cauliflower ear. Facial Plast Surg. 2010 Dec;26(6):451-5. doi: 10.1055/s-0030-1267719. Epub 2010 Nov 17. PMID: 21086231.
- Roy S, Smith LP. A novel technique for treating auricular hematomas in mixed martial artists (ultimate fighters). Am J Otolaryngol. 2010 Jan-Feb;31(1):21-4. doi: 10.1016/j.amjoto.2008.09.005. Epub 2009 Mar 26. PMID: 19944894.
- Kakarala K, Kieff DA. Bolsterless management for recurrent auricular hematomata. Laryngoscope. 2012 Jun;122(6):1235-7. doi: 10.1002/lary.23288. Epub 2012 Mar 22. PMID: 22447489.
- Brickman K, Adams DZ, Akpunonu P, Adams SS, Zohn SF, Guinness M. Acute management of auricular hematoma: a novel approach and retrospective review. Clin J Sport Med. 2013 Jul;23(4):321-3. doi: 10.1097/JSM.0b013e31825c4623. PMID: 22695406.
- Giles WC, Iverson KC, King JD, Hill FC, Woody EA, Bouknight AL. Incision and drainage followed by mattress suture repair of auricular hematoma. Laryngoscope. 2007 Dec;117(12):2097-9. doi: 10.1097/MLG.0b013e318145386c. PMID: 17921905.
- Malloy, Kelly Michele. Assessment and management of auricular hematoma and cauliflower ear. UpToDate, June 8, 2022.
- Photo credits for Figure 1 Boxer at Rest, adapted by cropping 07/14/2022 from open access Creative Commons, Carole Raddato Photographer 02/08/2014, https://www.flickr.com/photos/carolemage/13333237284/in/photostream/
- Other figures were created by author, patients involved gave full written consent complying with HIPAA guidelines.


Great article. I appreciated the clarification between the hematoma and the actual cauliflower ear. Also, very insightful as to potential causes for this issue seemingly to be “uncommon” to the medical community.
Thank you! Yeah it’s a pretty fascinating mechanism when it comes down to it isn’t it? See you on the mats.