Those who grapple have likely experienced some sort of mat funk either directly or indirectly. Mat funk is a nickname for a myriad of skin conditions that can occur from grappling, and given their different causes and thus different treatments they each deserve to be broken down and explained. This month’s post is on ringworm. Here are the quick bullets, but for a great deep dive, keep reading.
- Ringworm is caused by an infection from a fungus and not a worm.
- Ringworm, while very contagious, is typically not dangerous.
- Ringworm is easily treatable and preventable but it takes the efforts of the entire team.
Continue Reading: 10min Read
Overview and History
Ringworm isn’t actually a worm, it’s an infectious rash that is caused by one of a few fungi that love the skin. When these fungi cause an infection they spread outward from the original site and therefore one of the most common rashes seen is often circular and raised, or worm-like in appearance (see figure 1). It has been a known human disease and described for thousands of years and this was well before humanity knew of micro-organisms like fungi.
Given diseases were often named by the symptoms they caused, that’s how ringworm got it’s name. In fact it was called ‘tinea,’ which is latin for worm, and is thought to have started in the 2nd-3rd centuries.1 While tinea is still the dominant name used by medical professionals today, some will also use the term ‘dermatophytosis,’ because the fungi that cause this rash are broadly classified as dermatophytes, i.e. skin lovers.
Anatomy and Pathogenesis
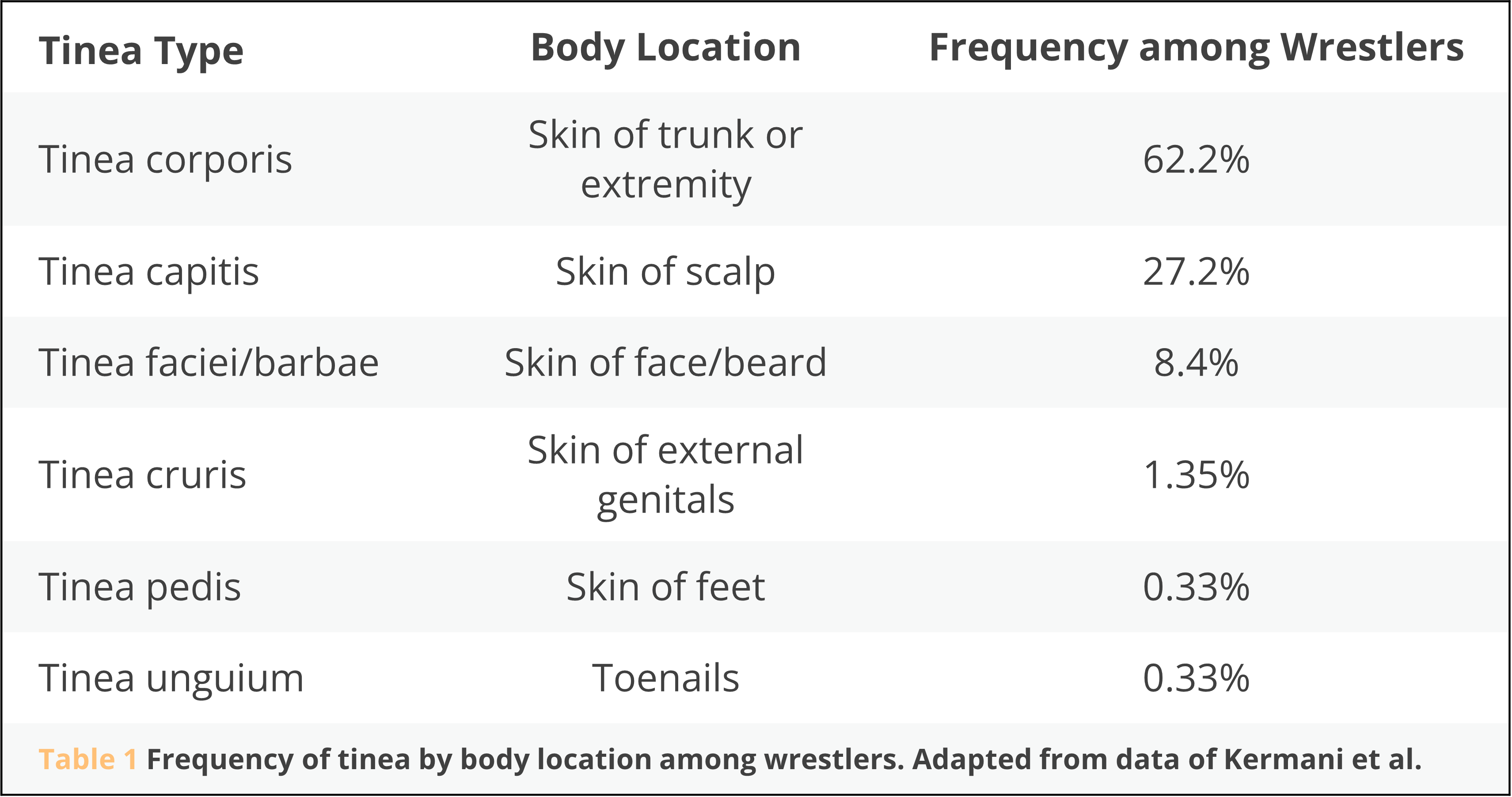
While highly contagious, it is not dangerous. Despite that, as many grapplers will attest, it is very annoying, usually itchy, and can cause hair loss if affecting a skin area with hair. Dermatophytes thrive on certain proteins that are located in the top layers of skin and can thus manifest most anywhere on the body where these layers exist. For research purposes, the medical literature defines a ringworm infection that was obtained by participating in contact sports as tinea gladiatorum (which is probably the best name for a disease ever). More importantly, as discussed further in the Treatment section, it is helpful for clinicians to further classify this infection by where exactly it is located on the body’s skin. For example, if it’s on the skin of the body tinea corporis, if it’s on the toenails it is called tinea unguium (a.k.a. onychomycosis), or if it’s on the beard area then tinea barbae (see Figure 2). Table 1 summarizes global data of the frequency of body locations infected by tinea gladiatorum specifically in wrestlers.2
Treatment
Despite the fungal cause of this infection first being described in 1837 and effective topical therapies being discovered in the mid-19th century, it wasn’t until 1958 that a safe and effective systemic therapy was first discovered.1 The infection can occur in any part of the skin, but if it infects the layers of skin deeper (e.g. hair follicles) than the most superficial layer then topical treatments are not effective as they cannot penetrate to the infection sufficiently. Thus while some ringworm infections will respond to topical therapy (e.g. tinea corporis, tinea pedis, etc) others will need anti-fungal pills in order to successfully treat them (e.g. tinea barbae, tinea unguium, etc).3,4 The good news is that most of the topical anti-fungals effective against ringworm are over-the-counter. While not as effective as the topical pharmacologics developed over the past sixty years, there is evidence that some topical herbal remedies, specifically tea tree oil for tinea pedis and oil of bitter orange for tinea corporis, can help as well.5,6 But one must use ‘natural’ herbal remedies with caution as their manufacturers are not held to the same production and testing standards as official pharmaceuticals. Some therefore can be unknowingly contaminated with toxins like heavy metals or they may not actually contain the active herbal ingredient they claim to have. In short, if you have a ringworm infection, there are safe and effective treatments available.
Prevention
Anybody who has dealt with a preventable disease would likely agree that ‘an ounce of prevention is worth a pound of cure.’ Ringworm and many of the other communicable skin conditions seen among grapplers are preventable. Many people point the blame and therefore their preventive measures at the gym mats, and while mat hygiene is important and essential in grappling sports, cleaning them after each use is only the tip of the iceberg of good gym hygiene. The reality is if there is even one person that has a contagious skin infection and rolls, it doesn’t matter how clean the mats are or how often they are cleaned. There will be a continuous source of infection that will constantly act as ‘patient zero’ for a gym. While it is true that mats and other shared equipment can harbor and possibly spread an infectious organism,7 evidence from a 2018 systematic review and meta-analysis of the best scientific literature available to date shows the prevalence of dermatophytes on wrestling equipment is roughly 5% vs being found on 34% of wrestlers themselves.2 If interested in a real life example, I’d recommend reading a compelling report from the CDC of an epidemiological investigation of skin infections following a 2014 wrestling tournament in Arizona.8 So as far as prevention measures go, I want to encourage first and foremost that if you are concerned about possibly having any skin infection don’t roll, and get it treated. If you are rash free, there is ample evidence in the medical literature that you can help the collective spread of all mat funk by washing/disinfecting your hands just prior to stepping on the mat,9 shower immediately after, and wash your gear after use.
Conclusion
Conclusion
I want to leave you with these departing words. If you get ringworm, nothing is wrong with you. Even following all the hygiene advice above, you may succumb one day to tinea gladiatorum. Microorganisms like dermatophytes live on our skin and often don’t even cause an infection. Remember, on average 34% of wrestlers worldwide will have it at any given time. I’ve had it, gotten it treated, and got back on the mat as soon as I could. So I encourage you to care for your team by caring for yourself.
References
- Negroni R. Historical aspects of dermatomycoses. Clin Dermatol. 2010 Mar 4;28(2):125-32. doi: 10.1016/j.clindermatol.2009.12.010. PMID: 20347652.
- Kermani F, Moosazadeh M, Hosseini SA, Bandalizadeh Z, Barzegari S, Shokohi T. Tinea Gladiatorum and Dermatophyte Contamination Among Wrestlers and in Wrestling Halls: A Systematic Review and Meta-analysis. Curr Microbiol. 2020 Apr;77(4):602-611. doi: 10.1007/s00284-019-01816-3. Epub 2019 Nov 26. PMID: 31773190.
- Goldstein A. Dermatophyte (tinea) Infections. In: UpToDate, Shefner JM (Ed), UpToDate, Waltham, MA. (Accessed here on June 30, 2022.)
- Boral H, Durdu M, Ilkit M. Majocchi’s granuloma: current perspectives. Infect Drug Resist. 2018 May 22;11:751-760. doi: 10.2147/IDR.S145027. PMID: 29861637; PMCID: PMC5968791.
- Martin KW, Ernst E. Herbal medicines for treatment of fungal infections: a systematic review of controlled clinical trials. Mycoses. 2004 Apr;47(3-4):87-92. doi: 10.1046/j.1439-0507.2003.00951.x. PMID: 15078424.
- Ernst E, Huntley A. Tea tree oil: a systematic review of randomized clinical trials. Forsch Komplementarmed Klass Naturheilkd. 2000 Feb;7(1):17-20. doi: 10.1159/000057164. PMID: 10800248.
- Hedayati MT, Afshar P, Shokohi T, Aghili R. A study on tinea gladiatorum in young wrestlers and dermatophyte contamination of wrestling mats from Sari, Iran. Br J Sports Med. 2007 May;41(5):332-4. doi: 10.1136/bjsm.2006.030718. Epub 2006 Nov 30. PMID: 17138633; PMCID: PMC2659067.
- Williams C, Wells J, Klein R, Sylvester T, Sunenshine R; Centers for Disease Control and Prevention (CDC). Notes from the field: outbreak of skin lesions among high school wrestlers–Arizona, 2014. MMWR Morb Mortal Wkly Rep. 2015 May 29;64(20):559-60. PMID: 26020140; PMCID: PMC4584520.
- Young LM, Motz VA, Markey ER, Young SC, Beaschler RE. Recommendations for Best Disinfectant Practices to Reduce the Spread of Infection via Wrestling Mats. J Athl Train. 2017 Feb;52(2):82-88. doi: 10.4085/1062-6050-52.1.02. Epub 2017 Jan 16. PMID: 28092165; PMCID: PMC5343532.
- Figures were created by author, patients involved gave full written consent complying with HIPAA guidelines.




Another great article. Great points on prevention from the individual perspective, which is where everyone has a part to play.
Thanks Jon! It was a fun write-up.